eMedicine Specialties > Pediatrics: General Medicine > Pulmonology
Atelectasis, Pulmonary
Updated: Sep 8, 2009
Introduction
Background
Atelectasis refers to collapse of part of the lung. It may include a lung subsegment or the entire lung and is almost always a secondary phenomenon, with no sex or race proclivities; however, it may occur more frequently in younger children than in older children and adolescents. The direct morbidity from atelectasis is transient hypoxemia due to blood flowing through the lung, which does not have normal air flow. The blood does not pick up oxygen from the corresponding alveoli. This shunting results in transient hypoxemia.
Pathophysiology
Atelectasis has 4 potential causes, which are as follows:
- Airways may have intrinsic obstruction.
- Airways may be compressed (extrinsic airway obstruction).
- Lung tissue may be compressed.
- Alveoli may incompletely expand and eventually collapse.
Because the right middle lobe orifice is the narrowest of the lobar orifices and because it is surrounded by lymphoid tissue, it is the most common lobe to become atelectatic. This is referred to as right middle lobe syndrome.
Intrinsic airway obstruction is the most common cause of atelectasis in children, and asthma is the most common underlying disorder that predisposes patients to atelectasis. Other causes include bronchiolitis, aspiration due to a swallowing disorder, endobronchial tuberculosis, aspiration from gastroesophageal reflux, airway foreign bodies, cystic fibrosis, and increased or abnormal airway secretions for other reasons. Children younger than 10 years are less likely to have developed the interairway canals of Lambert or the interalveolar pores of Kohn. Thus, young children depend more on the feeding airways to move air into the alveoli. When their airways become obstructed, they are more likely to develop atelectasis than older children who have developed those communications.
Extrinsic compression on the airways is most likely to come from enlarged lymph nodes (such as those due to tuberculosis infection), lymphoma and other tumors in the chest, an enlarged heart that compresses the left main or left lower lobe bronchus, and left-to-right intracardiac shunts that increase blood flow through the pulmonary arteries.
In children with hypoventilation for a protracted period, the alveoli may collapse. This may occur in children with neuromuscular disease, those who have had recent thoracic or upper abdominal surgery, those on medications that decrease their minute ventilation (such as narcotics), and those with abnormally small or dysmorphic chest walls, which may be less compliant than the normal chest wall. Such children may also be predisposed to atelectasis because of poor clearance of airway secretions. An ineffective cough allows these secretions to obstruct the airway.
Atelectasis due to compressed lung tissue occurs most commonly when air, blood, pus, or chyle is present in the pleural space. Intrathoracic abdominal contents, chest wall masses, cardiomegaly, and an abnormal chest wall can all compress adjacent lung tissue. If a portion of lung enlarges, such as with congenital emphysema, or if focal overinflation occurs for any other reason, it may compress the adjacent lung, causing atelectasis.
Frequency
United States
No data are available on the frequency of atelectasis.
Mortality/Morbidity
Most of the morbidity and any mortality is due to the underlying disorder. The primary complication of atelectasis is hypoxemia, which is usually transient. Within 24-48 hours, the lung is able to decrease or shut off blood flow to the atelectatic area. This is probably caused by factors such as serotonin that reacts to the local hypoxia in the alveoli and causes an intense vasoconstriction. If the atelectasis is massive enough, it may cause enough hypoxemia acutely to require supplemental oxygen or ventilatory support.
Atelectasis is a suggested cause of fever; however, no known physiologic reason supports this. Recent data dispute this old dogma. A study of adults after open-heart surgery showed no correlation between atelectasis and fever and reported that fever appeared as the incidence of atelectasis was decreasing.1 Patients with temperatures of more than 38.5°C were less likely to have atelectasis on radiography findings than those patients who were afebrile and undergoing radiography as part of the postoperative routine.
Another concern is the likelihood of infection in the atelectatic portion of the lung. Although the clearance in this portion of the lung is abnormal, the lung is normally a sterile environment. In the otherwise healthy child with atelectasis, infection is unlikely. However, if the child has abnormal secretions or is prone to aspiration, secondary infection of the atelectatic lung may occur. In children with chronically infected lungs, the atelectatic portion is likely to be similarly infected, with decreased ability to clear the infection. This sets up the possibility of bronchiectasis developing in that portion of the lung. Children who remain on assisted ventilation with atelectasis are at risk of developing infection, including infection in the atelectatic portion of the lung. This portion has less intrinsic clearance, which increases the risk of significant infection if organisms enter this portion.
Race
Other than any racial predilections for the underlying disorders, no racial predilection for atelectasis has been reported (see Cystic Fibrosis and Asthma).
Sex
Atelectasis has no sex predilection.
Age
Atelectasis is probably more common in children younger than 10 years because their airways are typically narrower and are more likely to become obstructed by secretions, airway inflammation, or both. In addition, these smaller airways are more easily compressed. These children are also less likely to have collateral ventilation.
Clinical
History
- Most symptoms of pulmonary atelectasis are related to the underlying disorder.
- Atelectasis alone only causes tachypnea as the child attempts to compensate for decreased tidal volume by increasing the frequency of respiration.
- If the atelectasis is large enough, the child may grunt in an attempt to create auto–positive end-expiratory pressure (PEEP), both to improve oxygenation and to attempt to open the atelectatic areas.
- If a child has underlying cardiopulmonary or neuromuscular disease and is on a monitor, sudden decreases in oxygen desaturation may be a sign of atelectasis. Atelectasis is one of the most common causes of sudden decreases in oxygen saturation in children.
Physical
- Most findings upon physical examination are related to the underlying disorder.
- Breath sounds may be decreased in the atelectatic portion of the lung, although the segment involved may be so small that the changes cannot be perceived. Also, the atelectatic portion may be in a segment inaccessible to the stethoscope.
- If the atelectatic portion and chest wall are large enough, dullness to percussion may be detected.
- The atelectasis may also occur in the right middle lobe or lingula in an adolescent girl. Because both are anteriorly located, the physician must listen to the anterior chest of the patient to hear these lobes. If the physician feels awkward about examining this area and fails to do so, the lobes are not correctly evaluated, and any corresponding abnormalities are not heard.
Causes
- Obstruction of an airway or diminished distention of alveoli may cause atelectasis.
- The most common causes involving airway obstruction include the following:
- Airway obstruction due to a mucous plug or other airway secretions, such as with bronchiolitis
- Bronchospasm airway secretions and airway inflammation in patients with asthma
- Abnormal airway secretions in cystic fibrosis
- Abnormal airway clearance, such as with ciliary dyskinesia syndrome
- Airway foreign body
- Extrinsic compression on an airway (eg, compression due to an enlarged or aberrant vessel)
- Enlarged lymph nodes that compress the airway
- Masses in the chest that compress the airway or alveoli
- Cardiomegaly or enlarged pulmonary vessels that compress adjacent airways
- Causes of diminished alveolar distention include the following:
- Small or dysmorphic chest wall
- Severe scoliosis
- Neuromuscular diseases
- Anesthesia or sedation
- Pain from upper abdominal surgery
- Abdominal distention
- Chest wall or upper abdominal pain
More on Atelectasis, Pulmonary |
 Overview: Atelectasis, Pulmonary Overview: Atelectasis, Pulmonary |
| Differential Diagnoses & Workup: Atelectasis, Pulmonary |
| Treatment & Medication: Atelectasis, Pulmonary |
| Follow-up: Atelectasis, Pulmonary |
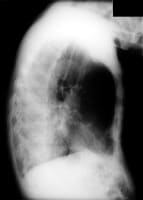
| Multimedia: Atelectasis, Pulmonary |
| References |
| Next Page » |
References
-
Engoren M. Lack of association between atelectasis and fever. Chest. Jan 1995;107(1):81-4. [Medline].
-
Bilan N, Galehgolab BA, Shoaran M. Medical treatment of lung collapse in children. Pak J Biol Sci. Mar 1 2009;12(5):467-9. [Medline].
-
[Guideline] National Heart, Lung and Blood Institute. Guidelines for the Diagnosis and Management of Asthma (EPR-3). [Full Text].
-
Bagley CE, Gray PH, Tudehope DI, Flenady V, Shearman AD, Lamont A. Routine neonatal postextubation chest physiotherapy: a randomized controlled trial. Journal of Paedtrics & Child Health. November 2005;41:592-7. [Medline].
-
De Boeck K, Willems T, Van Gysel D. Outcome after right middle lobe syndrome. Chest. Jul 1995;108(1):150-2. [Medline].
-
Finder J, Birnkrant DJ, Carl J et al. Respiratory care of the patient with Duchenne muscular dystrophy: An official ATS consensus statement. Am J Respir Crit Care Med. 2004;170:456.
-
Hendriks T, de Hoog M, Lequin MH, Devos AS, Merkus PJ. DNAse and atelectasis in non-cystic fibrosis pediatric patients. Critical Care. August 2005;9:351-6. [Medline].
-
Miske LJ, Hickey EM, Kolb SM, et al. Use of the mechanical in-exsufflator in pediatric patients with neuromuscular disease and impaired cough. Chest. Apr 2004;125(4):1406-12. [Medline].
-
Schindler MB. Treatment of atelectasis: where is the evidence?. Crit Care. Aug 2005;9(4):341-2. [Medline].
-
Slattery DM, Waltz DA, Denham B, et al. Bronchoscopically administered recombinant human DNase for lobar atelectasis in cystic fibrosis. Pediatr Pulmonol. May 2001;31(5):383-8. [Medline].
-
Stiller K. Physiotherapy in intensive care: towards an evidence-based practice. Chest. Dec 2000;118(6):1801-13. [Medline].
-
Woodring JH. Determining the cause of pulmonary atelectasis: a comparison of plain radiography and CT. AJR Am J Roentgenol. Apr 1988;150(4):757-63. [Medline].
-
Wu KH, Lin CF, Huang CJ, Chen CC. Rigid ventilation bronchoscopy under general anesthesia for treatment of pediatric pulmonary atelectasis caused by pneumonia: A review of 33 cases. Int Surg. Sep-Oct 2006;91(5):291-4. [Medline].
Further Reading
Keywords
lung, pulmonary collapse, collapsed lung, asthma, cystic fibrosis, CF, hypoxemia, extrinsic airway obstruction, intrinsic airway obstruction, bronchiolitis, aspiration from swallowing disorder, endobronchial tuberculosis, aspiration from gastroesophageal reflux, airway foreign bodies, increased airway secretions, enlarged lymph nodes, compressed lung tissue, pulmonary atelectasis, transient hypoxemia, lymphoma, hypoventilation, tachypnea, treatment, diagnosis