eMedicine Specialties > Radiology > Brain/Spine
Arachnoid Cyst Imaging: Imaging
Updated: Sep 21, 2009
- Overview
- Imaging
- Multimedia
Information from Industry
A BSN or MSN nursing degree prepares nurses with the knowledge and credentials needed to pursue new and emerging opportunities.
Explore career opportunities
Radiography
Plain radiographs have low sensitivity in the diagnosis of arachnoid cysts and contribute little to the diagnosis.
Intracranial
Forward bowing of the anterior cranial wall of the middle cranial fossa and elevation of the sphenoidal ridge have been reported findings on skull radiographs of patients with arachnoid cysts of the middle cranial fossa. However, such findings are difficult to assess; occasionally, patients with these features may be difficult to differentiate from normal patients. In addition, changes seen in other conditions, such as neurofibromatosis type I, may mimic these changes.
In infants, craniomegaly associated with widening of the fontanelle and thinning of the calvarium may be observed. However, these characteristics may be a normal variant and may be associated with other intracranial pathology.
Spinal
The spinal canal may be widened, and erosion of the pedicles may occur. However, the differential diagnosis is wide and includes spinal cord tumors.
Computed Tomography
There is a wide differential diagnosis for both intracranial and intraspinal cystic lesions, and arachnoid cysts have several mimics. In particular, with hemorrhagic arachnoid cysts, difficulties are encountered when the cyst contents are no longer isodense to CSF.
Intracranial
Intracranial arachnoid cysts may be an incidental finding on CT scans.
Typically, in cases of arachnoid cysts, the subarachnoid space is compressed by a cystic structure that may be unilocular or septate. The size of such structures varies. The septa may not always be visible (see the images below). The subjacent brain shows minimal mass effect.

Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the next image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.

Unenhanced CT scan of the head in a 26-year-old man with a history of seizures since childhood (same patient as in the previous image). The scan shows a large left frontoparietal cyst with a mass effect. The cyst was resected, and histologic analysis confirmed an arachnoid cyst.
On CT scans, arachnoid cysts are characterized by sharp, nonenhancing borders; they are isodense to CSF. On a bone window, remodeling of the skull may be evident. Arachnoid cysts seldom calcify.
On CT cisternography, arachnoid cysts may be seen to have a smooth outer surface, in contradistinction to epidermoid cysts, which typically have an irregular outer surface that is likened to the surface of cauliflower. With respect to cyst filling, CT cisternography yields mixed results. Some cysts fill with contrast immediately; with others, either filling is delayed or no filling occurs.
Noncommunicating and slow-filling cysts are regarded as true arachnoid cysts, whereas communicating cysts are regarded as diverticula of the subarachnoid space.
It has been proposed that noncommunicating cysts expand either as the result of a ball-valve mechanism or because of fluid secretion by the cyst wall, perhaps along an osmotic gradient.
Spinal
On CT scanning, spinal arachnoid cysts may not be sufficiently characterized to preclude the need for further imaging. CT scanning of the spine is useful in establishing the differential diagnosis of nondiscogenic radiculopathy; in addition, it demonstrates bone detail well.
Magnetic Resonance Imaging
MRI is the diagnostic procedure of choice in the detection of intracranial and intraspinal arachnoid cysts because of its potential to demonstrate the exact location and extent of the cysts and their relationship to the brain and spinal cord. The most important mimic of an arachnoid cyst is an epidermoid cyst.
Intracranial
On MRI, arachnoid cysts appear as well-defined nonenhancing intracranial masses that are isointense to CSF (see the images below).
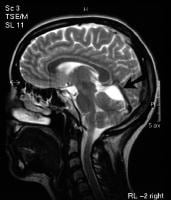
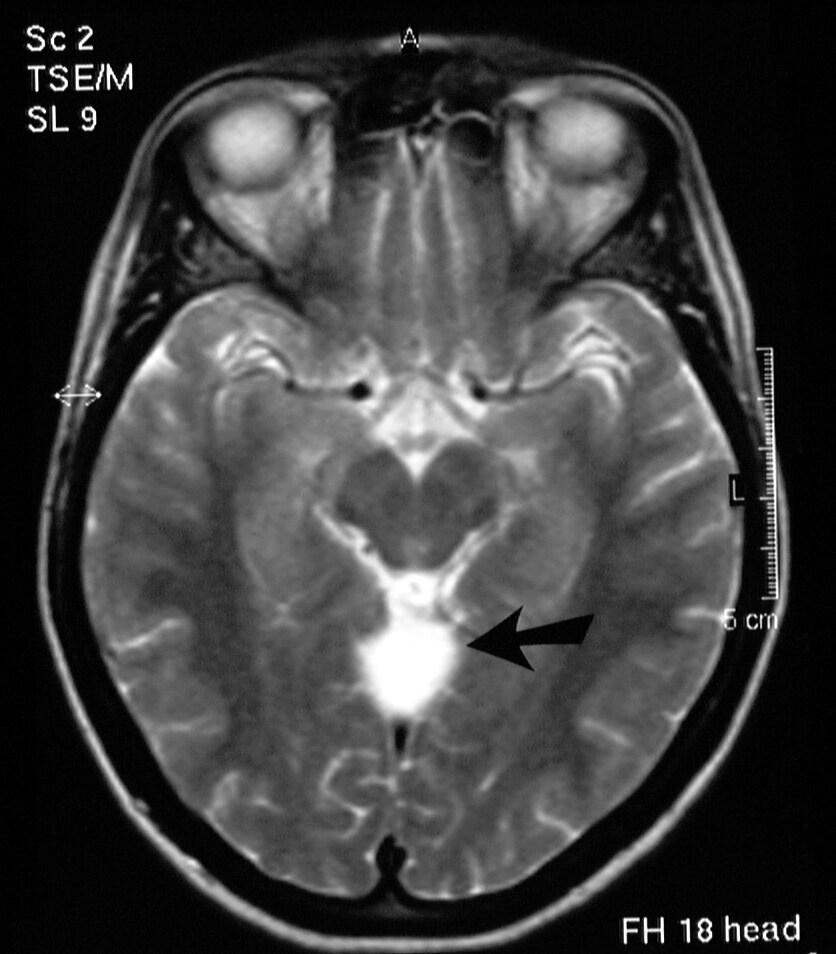
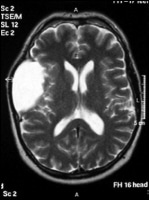
T2-weighted sagittal MRI image (see next image for axial view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).

T2-weighted axial MRI image (see previous image for sagittal view) of the brain in a 28-year-old woman with an incidental finding of a superior cerebellar cistern arachnoid cyst (arrow).

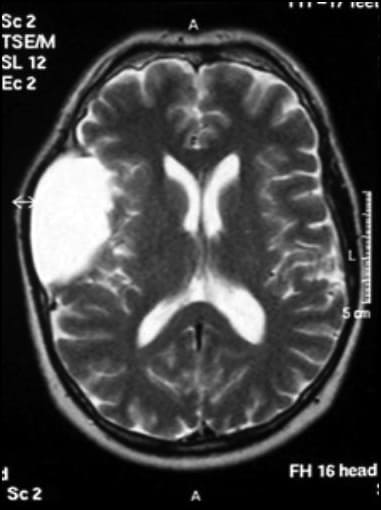
Axial T2-weighted MRI image through the midbrain, showing a right middle cranial fossa homogeneous lesion (same lesion as in the next 3 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.
Axial T2-weighted MRI image through the body of the lateral ventricles, showing superior extension of a right middle cranial fossa lesion. The lesion is homogeneous, with no perceptible wall, no internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
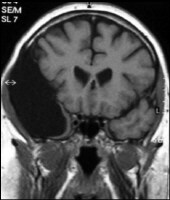
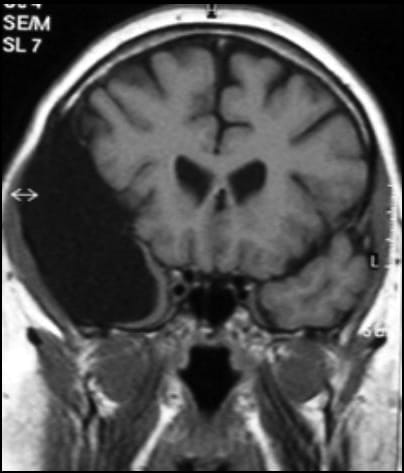
Coronal T1-weighted MRI image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent calvarium and brain displacement. These imaging features are typical of an arachnoid cyst.
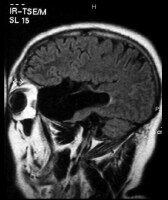
Sagittal fluid-attenuated inversion recovery (FLAIR) weighted image through a brain lesion, showing homogeneity of the lesion, lack of a perceptible wall, lack of internal complexity, and CSF signal intensity. There is associated remodeling of the adjacent sphenoid bone and brain displacement. These imaging features are typical of an arachnoid cyst.

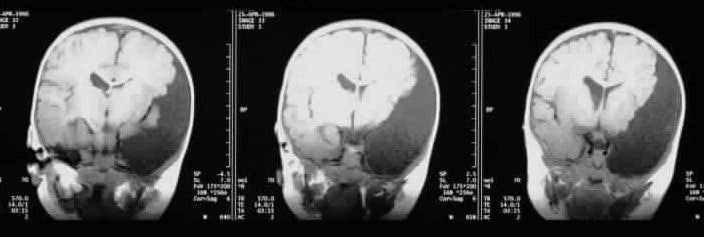
Prenatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion (postnatal images of same patient seen in the next 2 images) with CSF signal intensity and no perceptible wall or internal complexity. There is associated displacement of adjacent brain. These imaging features are typical of an arachnoid cyst.

Postnatal coronal T2-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
Postnatal coronal T1-weighted MRI images through the middle cranial fossa, showing a left temporal fossa homogeneous lesion with CSF signal intensity and no perceptible wall or internal complexity. There is associated remodeling of adjacent calvarium, brain displacement, and a midline shift. These imaging features are typical of an arachnoid cyst.
Diagnostic confusion occasionally arises between arachnoid cysts and epidermoid cysts. The 2 masses may have similar characteristics on T1-weighted and T2-weighted images, and neither shows enhancement with gadolinium. However, arachnoid cysts follow CSF signals on all sequences—in particular, on the FLAIR sequence—in contradistinction to epidermoid cysts. DWIs allow easier differentiation of the 2 masses.
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Systemic Fibrosis. The disease has occurred in patients with moderate to end-stage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans.
NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see Medscape.
As a result of the CSF contents of arachnoid cysts, the signal intensity on DWI is low; epidermoid cysts tend to have a high signal on DWI.
Some arachnoid cysts contain proteinaceous fluid or blood. In such cases, signal loss on DWI may not be marked; this may pose diagnostic problems when using DWI.
FLAIR imaging demonstrates tissue contrast similar to that of T2-weighted images, but FLAIR shows no signal arising from the CSF. Therefore, FLAIR demonstrates a suppressed (low) signal in arachnoid cysts that contain CSF; in epidermoid cysts, that signal is typically higher.
A large cisterna magna (mega cisterna magna) occasionally may be confused with an arachnoid cyst. Mega cisterna magna may represent a normal variant (intact cerebellum and vermis), but it may be associated with Dandy-Walker syndrome, either full blown or a variant in which the vermis is either completely or partially absent. Mega cisterna magna and arachnoid cysts show CSF characteristics on T1-weighted, T2-weighted, DWI, and FLAIR sequences. However, whereas an arachnoid cyst may demonstrate mass effect with an en bloc displacement of the cerebellum and vermis, normal-variant mega cisterna magna demonstrates no mass effect, and the cerebellum and vermis remain intact.
Spinal
MRI of spinal arachnoid cysts demonstrates an oval, sharply demarcated extramedullary mass that may cause local displacement and/or spinal cord compression.
The cyst is usually hyperintense to CSF on T2-weighted sequences because of the relative lack of CSF pulsation artifacts.6,7,8,9
Ultrasonography
Ultrasonography has a high yield in the detection and characterization of cystic masses. Cranial ultrasonography is an important diagnostic tool during the first year of life. However, it is limited by the closure of the anterior fontanelle, which normally occurs in full-term infants 9-18 months of age.
Intracranial cysts and ventriculomegaly also may be detected and characterized by transcranial ultrasonography through a burr hole.10
Angiography
Findings on angiography indicate that there is a higher incidence of an absence of the middle cerebral vein in patients with arachnoid cysts of the middle fossa, as compared with the general population.
Angiographic findings indicate that among patients with arachnoid cysts of the middle fossa, there is a decrease in drainage of the middle cerebral vein into the cavernous sinus on the side of the cyst.
More on Arachnoid Cyst Imaging |
| Overview: Arachnoid Cyst Imaging |
 Imaging: Arachnoid Cyst Imaging Imaging: Arachnoid Cyst Imaging |
| Multimedia: Arachnoid Cyst Imaging |
| References |
| « Previous Page | Next Page » |
References
-
Van Tassel P, Cure JK. Nonneoplastic intracranial cysts and cystic lesions. Semin Ultrasound CT MR. Jun 1995;16(3):186-211. [Medline].
-
Algin O, Hakyemez B, Gokalp G, Korfali E, Parlak M. Phase-contrast cine MRI versus MR cisternography on the evaluation of the communication between intraventricular arachnoid cysts and neighbouring cerebrospinal fluid spaces. Neuroradiology. May 2009;51(5):305-12. [Medline].
-
Hughes G, Ugokwe K, Benzel EC. A review of spinal arachnoid cysts. Cleve Clin J Med. Apr 2008;75(4):311-5. [Medline].
-
Tsutsumi S, Kondo A, Yasumoto Y, Ito M. Asymptomatic huge congenital arachnoid cyst successfully treated by endoscopic surgery--case report. Neurol Med Chir (Tokyo). Sep 2008;48(9):405-8. [Medline].
-
Zeng L, Feng L, Wang J, Li J, Wang Y, Chen J, et al. Comparative study on two surgical procedures for middle cranial fossa arachnoid cysts. J Huazhong Univ Sci Technolog Med Sci. Aug 2008;28(4):431-4. [Medline].
-
Kollias SS, Bernays RL. Interactive magnetic resonance imaging-guided management of intracranial cystic lesions by using an open magnetic resonance imaging system. J Neurosurg. Jul 2001;95(1):15-23. [Medline].
-
Hu XY, Hu CH, Fang XM, Cui L, Zhang QH. Intraparenchymal epidermoid cysts in the brain: diagnostic value of MR diffusion-weighted imaging. Clin Radiol. Jul 2008;63(7):813-8. [Medline].
-
Secer HI, Anik I, Celik E, Daneyemez MK, Gonul E. Spinal hydatid cyst mimicking arachnoid cyst on magnetic resonance imaging. J Spinal Cord Med. 2008;31(1):106-8. [Medline].
-
Herman-Sucharska I, Urbanik A. [MRI of fetal central nervous system malformations]. Przegl Lek. 2007;64(11):917-22. [Medline].
-
Slovis TL, Canady A, Touchette A, Goldstein A. Transcranial sonography through the burr hole for detection of ventriculomegaly. A preliminary report. J Ultrasound Med. Apr 1991;10(4):195-200. [Medline].
Further Reading
Keywords
arachnoid cyst, glioependymal cyst, meningeal cyst, intra-arachnoid cerebrospinal fluid–containing cysts, intracranial mass, leptomeningitis, arachnoid diverticula, spinal arachnoid cysts
Contributor Information and Disclosures
Author
Ali Nawaz Khan, MBBS, FRCS, FRCP, FRCR, Consultant Radiologist and Honorary Professor, North Manchester General Hospital Pennine Acute NHS Trust, UK
Ali Nawaz Khan, MBBS, FRCS, FRCP, FRCR is a member of the following medical societies: American Association for the Advancement of Science, American Institute of Ultrasound in Medicine, British Medical Association, British Society of Interventional Radiology, Royal College of Physicians, Royal College of Physicians and Surgeons of the United States, Royal College of Radiologists, and Royal College of Surgeons of England
Disclosure: Nothing to disclose.
Coauthor(s)
Ian Turnbull, MB, ChB, MD, DMRD, FRCR, Lecturer, Department of Radiology, University of Manchester; Consulting Neuroradiologist, Hope Hospital, Salford, Manchester and North Manchester General Hospital, UK
Disclosure: Nothing to disclose.
Riyadh Al-Okaili, MBBS, Interventional/Therapeutic and Diagnostic Neuro-Radiologist, King Abdulaziz Medical City
Riyadh Al-Okaili, MBBS is a member of the following medical societies: American College of Radiology
Disclosure: Nothing to disclose.
Sumaira MacDonald, MBChB, PhD, MRCP, FRCR, Lecturer, Sheffield University Medical School; Endovascular Fellow, Sheffield Vascular Institute
Sumaira MacDonald, MBChB, PhD, MRCP, FRCR is a member of the following medical societies: British Medical Association, Royal College of Physicians, and Royal College of Radiologists
Disclosure: Nothing to disclose.
Khalid Mahmood, MBBS, FCPS, Locum Appointment Training Specialist Registrar, Department of Radiology - Paediatric, Royal Liverpool (Alder Hey) Children's Hospital
Disclosure: Nothing to disclose.
Medical Editor
Lucien M Levy, MD, PhD, Director of Neuroradiology, Professor of Radiology, Department of Radiology, George Washington University Medical Center
Lucien M Levy, MD, PhD is a member of the following medical societies: American Cancer Society, American College of Radiology, American Heart Association, American Medical Association, American Roentgen Ray Society, American Society of Neuroradiology, and Radiological Society of North America
Disclosure: Nothing to disclose.
Pharmacy Editor
Bernard D Coombs, MB, ChB, PhD, Consulting Staff, Department of Specialist Rehabilitation Services, Hutt Valley District Health Board, New Zealand
Disclosure: Nothing to disclose.
CME Editor
Robert M Krasny, MD, Resolution Imaging Medical Corporation
Robert M Krasny, MD is a member of the following medical societies: American Roentgen Ray Society and Radiological Society of North America
Disclosure: Nothing to disclose.
Chief Editor
James G Smirniotopoulos, MD, Professor of Radiology, Neurology, and Biomedical Informatics; Program Director, Diagnostic Imaging Program, Center for Neuroscience and Regenerative Medicine (CNRM), Uniformed Services University of the Health Sciences
James G Smirniotopoulos, MD is a member of the following medical societies: American College of Radiology, American Roentgen Ray Society, American Society of Head and Neck Radiology, American Society of Neuroradiology, American Society of Pediatric Neuroradiology, Association of University Radiologists, and Radiological Society of North America
Disclosure: Nothing to disclose.