Bicuspid Aortic Disease
Below you will find information regarding the following topics:
- Bicuspid Aortic Disease
- Bicuspid Aortic Valve
- Bicuspid Aortic Valve Insufficiency (Regurgitation)
- Bicuspid Aortic Valve Stenosis
- The Aorta, Heart and Other Organs
- Variations in Disease Expression
- Diagnosis and Treatment
- For More Information and Appointments
Bicuspid Aortic Disease
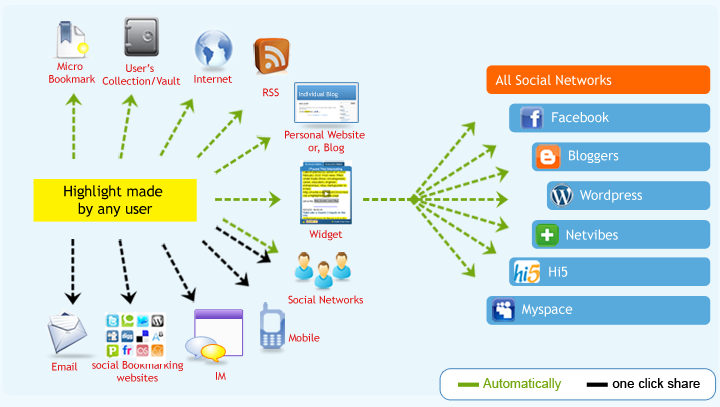
Aortic valve malformation is the most recognized aspect of a congenital condition now known to potentially affect not only the aortic valve, but also the tissue of the aorta and other heart structures and organs. Bicuspid aortic disease (BAD) refers to the condition in its entirety, including the existence of some combination of the following:
- Bicuspid aortic valve (BAV)
- Aortic dilation, aneurysm or dissection (most commonly involving ascending aorta)
- Other miscellaneous degenerative affects
- Labile hypertension (rapid change with activity or stress)
Bicuspid Aortic Valve
The bicuspid aortic valve is the most common congenital heart defect. It is estimated to exist in 1 to 2 % of the population, predominating in males.
 The normal aortic valve, as shown in the drawing, has three leaflets (flaps, cusps) that move flexibly, opening and closing to control the flow of blood into the aorta from the left ventricle of the heart as it beats. When the cusps come together as the valve closes, the shape is that of a trisected circle.
The normal aortic valve, as shown in the drawing, has three leaflets (flaps, cusps) that move flexibly, opening and closing to control the flow of blood into the aorta from the left ventricle of the heart as it beats. When the cusps come together as the valve closes, the shape is that of a trisected circle.
(Click on image to view aortic valve.)
In contrast, a BAV has only two leaflets, also shown in the diagram on the left. It is sometimes described as resembling the mouth of a fish as it opens and closes. Depending on the degree of malformation and associated malfunction, blood flowing through the valve may make an abnormal sound, called a murmur. While some bicuspid aortic valves are silent, the detection of a murmur may be the first indication of abnormality of the aortic valve.
Over time a bicuspid valve may lose its ability to open widely, close properly or both. As previously described, a murmur may develop. Regardless of how the valve is failing, it should be monitored and a surgical solution planned appropriately before any lasting damage is done to the heart.
Bicuspid Aortic Valve Insufficiency (Regurgitation)
If the cusps (leaflets) of the valve fail to come together tightly when closing, blood leaks back into the heart. Either of two terms may be used to describe this leakage: insufficiency or regurgitation. Depending on its severity, this condition may place a strain on the heart, which is forced to re-pump the additional backflow of blood (overloaded left ventricle). In time an overloaded ventricle may have permanent stretching of the muscle fibers, and even if corrective surgery is done may not fully regain its pumping efficiency.
Bicuspid Aortic Valve Stenosis
Some bicuspid aortic valves lose the ability to open widely and often have calcium deposits on the cusps. This condition is called stenosis. As the valve opening becomes narrower, the heart must work harder to force blood through the small opening. This stresses the heart, and with time the wall of the left ventricle may thicken (over pressurized heart). As a result the heart is unable to relax during diastole, and the heart muscle becomes very stiff and inefficient (diastolic dysfunction).
The Aorta, Heart and Other Organs
Other distinctive features of bicuspid aortic disease (BAD) may be seen in the heart, where the mitral valve may also be regurgitant as a result of myxomatous changes. While the pulmonary valve often functions well, its use as an aortic autograft in the Ross procedure is controversial due to concerns regarding the underlying connective tissue. On a positive note, the coronary arteries, which supply blood to the heart, are usually clear and free of blockages, unless there is a history of smoking or other associated risk factors, such as hypercholesteremia, diabetes, previous heart attack or atherosclerosis.
The tissue of the aortic wall may be abnormal due to a degenerative process in the medial layer of the aorta. This results in a weakened, thin aorta that is unable to stretch and contract properly. The aortic tissue is prone to aneurysm formation and/or dissection.
 In BAD, this is particularly true of the ascending aorta with extension into the arch. Medical treatment and elective surgery are important in avoiding serious, life-threatening events. Signs of degenerative disease may exist in other blood vessels and organs. Examples of this are subclavian or renal artery aneurysms, cysts in the kidneys and liver, hiatal hernias and effects on the eyes resulting in poor vision.
In BAD, this is particularly true of the ascending aorta with extension into the arch. Medical treatment and elective surgery are important in avoiding serious, life-threatening events. Signs of degenerative disease may exist in other blood vessels and organs. Examples of this are subclavian or renal artery aneurysms, cysts in the kidneys and liver, hiatal hernias and effects on the eyes resulting in poor vision.
(Click on image to view ascending aortic aneurysm.)
Variations in Disease Expression
While the bicuspid aortic valve itself is well known, information about the broader implications of this disease is still emerging, making the search for comprehensive information and expert treatment a challenging one. Understanding the nature of this condition and its potential affect on the aorta is crucial to the safety and longevity of those affected by it.
Bicuspid aortic disease is a condition that exists at birth. There can be significant variation in the way individuals are affected. However, the aortic root and ascending aorta are the aortic segments most commonly involved, and they are generally larger when compared to those in similar patients with normal trileaflet aortic valves. It is also known that development of aortic aneurysm or dissection may occur whether or not the bicuspid aortic valve has been replaced. Although it is possible to live a normal life span without experiencing problems due to this condition, many bicuspid disease individuals will require treatment during their lifetime. While the stereotypical patient requiring treatment might be a male in his 50s, this condition occurs across a broad range of ages in both males and females. Young individuals with bicuspid aortic valve regurgitation (leaking) experience a higher rate of dissection, aneurysm formation and rupture of the aorta, indicating a more severe form of the disease.
Bicuspid aortic disease has been found to affect multiple family members across generations, which has prompted research into the genetic aspects of this condition. Information emerging from these studies indicates that in families with bicuspid aortic disease, some members may develop ascending aortic aneurysm although the aortic valve appears normal. This condition also may skip generations, and since it is not possible to predict who may be affected, it is important to monitor all family members. This includes parents, children, brothers or sisters and extended family such as nephews, nieces and grandchildren.
Currently there are no tests capable of determining who will experience failure of the valve, aortic aneurysm or aortic dissection. However, the latest advances in understanding this condition have enabled development of a treatment plan for this subset of patients. Proactive patient education and diagnostic monitoring, along with early medical treatment and lifestyle modifications at the first sign of disease, are key to the successful management of this condition. The Thoracic Aortic Surgery Program includes a liaison who works with our patients and families. Anyone with questions or concerns is welcome to contact the liaison regarding bicuspid aortic disease.
Diagnosis and Treatment
Diagnostic Tests
Various diagnostic tests are performed to monitor the status of both the aorta and the aortic valve over time. They also provide information regarding the other valves and chambers of the heart. The main diagnostic tests involved are echocardiograms, CT scans and MRIs. Nuclear medicine tests (adenosine, thallium) may be used to determine whether coronary artery blockage is also present. Other tests including ultrasound examination of the carotid arteries, chest X-rays and routine blood tests are also performed prior to surgery.
Medical Treatment
Medical treatment for both the enlarged aorta and regurgitant aortic valve, in the absence of congestive heart failure, is similar. This consists of blood pressure medications (ACE inhibitors, ARBs and calcium channel blockers) and beta blockers. The goal of this treatment is to slow the enlargement of the aorta, reduce the risk of rupture or dissection of the aortic tissue and minimize the backflow of blood through the valve. In the presence of congestive heart failure, a diuretic and possibly digoxin may be added along with modification of the beta blocker dosage. As a general guideline, prior to surgery systolic blood pressure is medically maintained in a range between 105 and 110 during normal activity.
Lifestyle recommendations include diet, exercise, and smoking cessation. Patients should not smoke either actively or passively. Weight management and diet modifications include a diet that is low in fat and carbohydrates and high in protein and fiber. Exercise is helpful and strongly encouraged, including power walks of 15 to 30 minutes two to three times daily. However, heavy lifting is prohibited due to the pressure it exerts on the aorta.
Surgical Treatment
The objective of aortic surgery is to provide a stable long-term solution. The durability of commercial Dacron aortic grafts available today for aortic replacement exceeds the human life span. If replacement of the bicuspid aortic valve is necessary, proven state-of-the-art valves appropriate to the patient's overall condition, lifestyle and age are recommended. Elective surgery is suggested to replace the failing bicuspid aortic valve before any lasting damage is done to the heart. In conjunction with this, surgical options exist for the aortic root and ascending aorta to proactively prevent future dissection or aneurysm formation.
Surgery on the aorta is recommended when the risk of aortic rupture or dissection is greater than the risk of surgery. In situations where the aorta requires surgery and the aortic valve has already been replaced or is still working normally, the valve may be spared and only the diseased portions of the aortic root and ascending aorta replaced. Replacement may also include part or all of the aortic arch. For further details regarding surgical options please see the web page.
Ongoing Postsurgical Care
Following surgery, ongoing medical treatment is aimed at protecting the graft, the remaining aorta, the aortic valve, and the cardiovascular system generally. Diagnostic tests are also performed at prescribed intervals.
Infection Prevention
For patients with bicuspid aortic disease, as with any cardiac valve disease, antibiotic treatment for the prevention of infection is extremely important and must be taken seriously. It is generally well understood that antibiotic treatment is required prior to teeth cleaning and all other dental procedures. However, it is important that antibiotic pre-treatment be given prior to any invasive procedure. The skin provides a natural barrier to infection, and anything that penetrates that barrier introduces the risk of infection. Procedures such as a breast biopsy, removal of an ingrown toenail or a wart on the hand, a simple hernia repair or an angiogram/heart catheterization are all examples of invasive procedures requiring pre-treatment.
It is important for the patient to inform all medical professionals involved with any procedure about their valve and/or aortic condition. The patient's cardiac care providers should be contacted with any questions prior to any invasive procedures. In some cases, oral antibiotics may not be sufficient, and intravenous antibiotic therapy may be required. Endocarditis is a severe infection that is difficult to treat and potentially life threatening. It is important that all possible steps are taken to prevent it.
Anticoagulation Therapy
Those with a bioprosthesis or an autograft in the aortic position typically do not require long-term anticoagulation with Coumadin. The exceptions are those patients who remain in atrial fibrillation for more than 72 hours. Aspirin therapy may be given, if aspirin is tolerated. Anyone with a mechanical prosthesis in the aortic position requires full anticoagulation with Coumadin. The level of anticoagulation is monitored by periodic PT/INR measurements. The desired PT/INR recommended may vary slightly depending on the particular valve implanted, but typically a range of 2.4 to 2.8 for the INR is desirable. Persantine or baby aspirin may also be given as anti-platelet therapy. Devices are now available for in-home monitoring of the PT/INR. These devices have proven beneficial to patients in significantly decreasing the incidence of bleeding complications due to incidentally prolonged PT/INR values that are secondary to dietary changes.
For More Information and Appointments
To view some frequently asked questions about bicuspid aortic disease, click here. For additional information, please contact:
| Thoracic Aortic Surgery Program |
| Cedars-Sinai Medical Center |
| 8700 Beverly Blvd., Suite 6215 |
| Los Angeles, CA 90048 |
| Phone: 1-800-CEDARS-1 (233-2771) |
| Fax: (310) 423-0127 |
| Send Us a Message |
Appointments may also be scheduled with the Thoracic Aortic Surgery Program either by phone or e-mail. To request an appointment for a consultation, contact:
| Division of Cardiothoracic Surgery |
| Phone: (310) 423-3851 |


























Connect with us